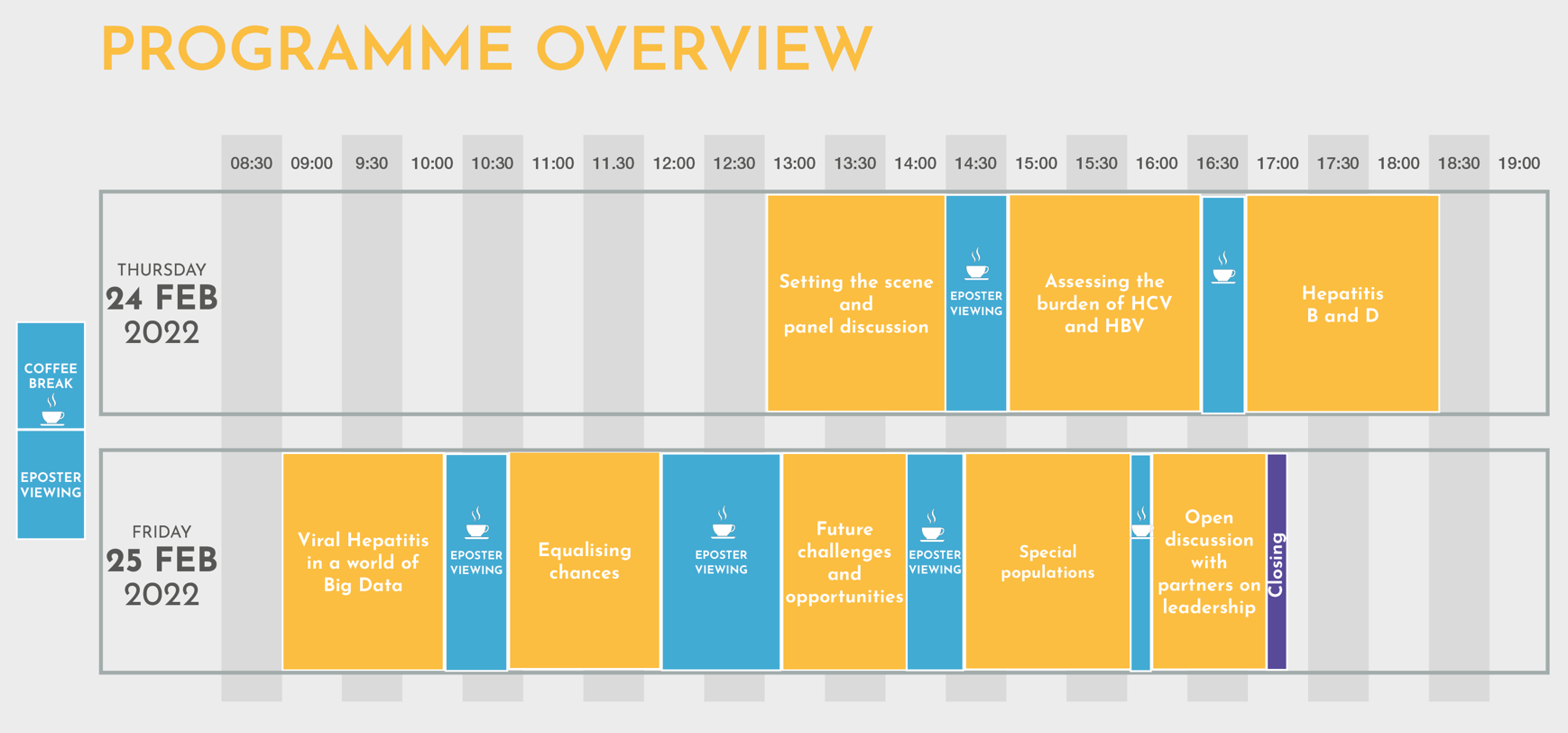
Session 1: Introduction and aims of the conference
The WHO goal of eliminating viral hepatitis has led to a surge in activities to achieve a world free from viral liver disease. International experts will discuss optimal approaches to eliminate viral liver disease and to assess progress towards elimination. The conference will aim to provide guidance and recommendations to those working towards elimination of hepatitis b and hepatitis C.
Session 2: Assessing the burden of hepatitis B and C
This session will provide a critical assessment of the methodology currently used to measure incidence, prevalence, and health burden (both morbidity and mortality) of viral hepatitis. In particular, during a dedicated panel discussion, both model-based and population sampling-based estimates will be compared, and their advantages and limitations critically analysed. An additional discussion will be devoted to the clinical impact of comorbidities in patients both living with chronic hepatitis B and taking antiviral therapy.
Session 3: Hepatitis B and D
Transmission of the hepatitis B virus (HBV) occurs mainly perinatally and during early childhood in highly endemic areas, but more often by sexual contact or through contaminated needles in low endemic areas. Universal vaccination of all infants as soon as possible after birth (preferably within 24 hours, followed by two or three doses, four weeks apart) is the most feasible and cost-effective strategy for HBV infection control. Furthermore, the HBV vaccine is the mainstay of both hepatitis B and D prevention. According to WHO estimates, the proportion of children under five years of age chronically infected with HBV dropped to just under 1% in 2019, down considerably from around 5% in the pre-vaccine era (ranging from the 1980s to the early 2000s). This marks the achievement of one of the milestone targets to eliminate viral hepatitis in the Sustainable Development Goals.
However, the coverage of HBV vaccine at birth remains uneven. It is particularly low in the African region, where the HBV burden is currently higher, thus alternative policies to overcome the barriers to vaccination need to be identified. Antiviral therapy serves to limit HBV infection spreading from highly viremic HBsAg-positive mothers and in the setting of high-risk groups (such as prisoners, people who inject drugs, and people with multiple sex partners). Individualised antiviral therapy, however, is currently an unmet need. New algorithms and/or models of circulating biomarkers to simulate the dynamics of the HBV and host interplay and to tailor different combinations of antiviral drugs to the different clinic-pathologic conditions of the individual patient need to be developed. Likewise, surrogate markers of off-treatment sustained response are needed to enable a safe withdrawal of treatment. In patients with chronic hepatitis D, it is essential to identify key HBV helper functions (such as viral proteins production vs viral replication) as target of antiviral therapy, in order to reach optimal control of both HBV and HDV infections.
Session 4. Viral Hepatitis in a world of big data
This session will explore the multifaceted issue of data in the context of hepatitis elimination. High-quality data on viral hepatitis is scarce and there is a need for better-quality data to improve patients’ health outcomes. Factors such as the privacy and security of this data must also be guaranteed. In this session, data collection, both at European level and internationally, will be discussed as well as the opportunities and challenges relating to a uniform European-wide collection system. One discussion will focus on vulnerable populations who are most heavily affected by hepatitis, such as people living in institutions, and pregnant women and their infants. Collecting data is critical to improve health in these populations, but data collection should be designed in a thoughtful manner that does not inadvertently harm vulnerable populations.
Session 5: Equalising chances
This session will address several aspects of inequalities with regards to viral hepatitis elimination such as reasons for multiple treatment failure or impact of stigmatisation on acceptance of viral hepatitis diagnosis. The road to an HCV vaccine will also be explored as one of the responses to viral hepatitis elimination. Finally, the management of children with viral hepatitis is going to be adressed.
Session 6: Future challenges and opportunities
The general discussion will be on the industry-led initiatives to facilitate access to medicines, especially in underserved settings. The aim would be to find responses to the challenging questions such as how industries can please both shareholders and the needs of the underserved countries.
Moreover, panellists will highlight what is the role of industries in the education of physicians and patients. They will provide the public with their advocacy initiatives and interactions with policymakers and related inquiries and opportunities.
Session 7: Special populations
Viral hepatitis disproportionally affects the most vulnerable, marginalised, and underserved populations. As they often face the greatest challenges in accessing necessary services, because of social and structural barriers, these populations are often lost to follow-up along the continuum of care and have underserved health outcomes. Moreover, the marginalisation of key populations heightens the epidemic and diminishes efforts towards the WHO goal of elimination of viral hepatitis by 2030. This session will address pressing gaps and potential solutions for these populations, such as the managing of viral hepatitis in migrants and expanding the provision of hepatitis C services for men who have sex with men. Further, the session will explore how to reach the population of former drug users, and the possibilities of eliminating viral hepatitis in prisons.
Session 8: Open discussion with partners on leadership in awareness raising, advocacy, and efforts towards viral hepatitis elimination
To overcome the barriers to achieving viral hepatitis elimination, we must improve people’s access to treatment and care. To this end, all actors involved, including patient organisations, must work together and deliver care at the community level. In this session, we will discuss with key patient associations (Coalition for Global Hepatitis Elimination, Correlation Network, European Liver Patients’ Association, European Monitoring Centre for Drugs and Drug Addiction, Liver Patients International, World Hepatitis Alliance) their efforts towards viral hepatitis elimination and access to care and how European authorities (WHO Europe, European Centre for Disease Prevention and Control, and the European Commission) may help.